Care You Need, When You Need It
Get health tips, treatment, and evaluation on your schedule with Baptist Health.
Find a Provider
Reviewed by: Michael Newkirk, MD
Last updated: November 19, 2020
The COVID-19 pandemic has turned words like social distancing and pandemic into household terminology. Now, as we inch closer to a potential treatment for the virus that has rocked the world, a new word is spurring much interest and intrigue: antibodies.
Specialized, Y-shaped proteins that are made by the immune system to fight infections, are called antibodies by binding to the viruses or bacteria. As part of the “adaptive” immune system, antibodies may also prevent future infections from the same illnesses by allowing the immune system to recognize and rid specific pathogens.
Also called immunoglobulins (Ig), antibodies come in a few different shapes and sizes, but pretty much have the same basic Y-shape, with five variations called IgG, IgM, IgA, IgD, and IgE with a slightly varying role to the immune system.
In terms of development, antibodies can take days or weeks to develop in the body following exposure to an infection and it is unknown how long they stay in the blood.
When foreign substances like bacteria or viruses enter your body, the immune system recognizes it as a threat and responds with an attack in an attempt to keep your body healthy.
The bacteria or virus that enters your body has markers on its surface called antigens. When your body encounters these antigens for the first time, specialized white blood cells in your immune system called B Cells create a counter-attack in the form of antibodies. These antibodies are created to specifically target the antigen that prompted the immune response.
Antibodies travel through the bloodstream searching out the antigens from the foreign substance and binding to them upon contact. Once bound, antibodies destroy the antigens, and your body continues creating antibodies until the bacteria or virus that invaded your body is eliminated.
Some antibodies stay in your immune system after the antigens they fought against are long gone. Thus, if you are exposed to the same bacteria or virus again, those antibodies can re-engage to protect you from the illness again. Essentially, these antibodies can provide immunity from infection for a period of time post initial exposure.
Antibodies can take days to weeks to develop after exposure to SARS-CoV-2, the virus that causes COVID-19. It is unknown how long they stay in the blood to provide benefit to subsequent exposures.
Antibodies can work to combat an active infection, and in some cases, can prevent infection. While incredibly valuable, antibody treatment is not the same as a vaccine.
A vaccine contains a part of the actual virus – either an inactive part of the virus, or a live virus that cannot cause infection. Exposure to this part of the virus causes the body to naturally produce antibodies in response to the vaccine, thus warding off the virus and providing immunity to future exposures.
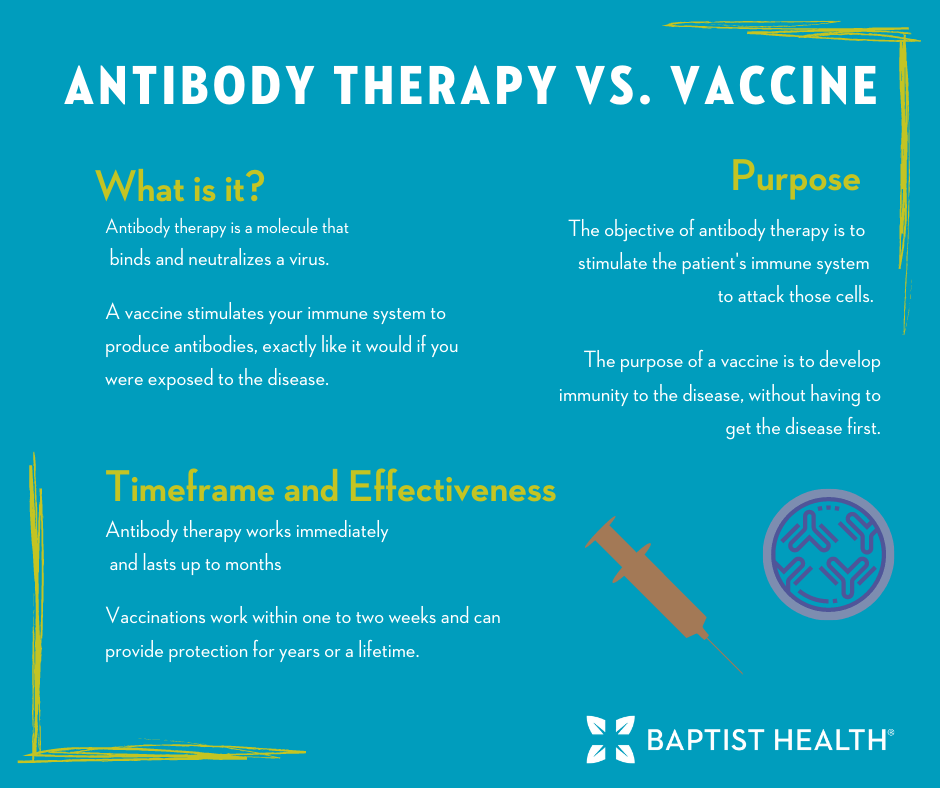
Vaccines work for future protection against disease but are not an effective treatment for someone who is already ill. Antibody therapy can often produce faster results than vaccines, which generally take longer to provide protection. Antibody therapy can be a good alternative for treatment and prevention in people who do not respond well to vaccines. A good example of this is the elderly, who are particularly vulnerable to the effects of COVID-19.
Overall, vaccines are a better long-term protection than antibody therapy. Vaccines can provide protection for years, or in some cases a lifetime, while antibody therapy may provide immunity for only weeks to months. Vaccines are also easier to administer and more cost-effective.
At the time of submission for this post, Baptist Health has initially received 250 doses of the bamlanivimab antibody drug that are being distributed to our nine hospitals in proportion to the number of COVID-19 patients they are treating and the size of the facility.
We’re finalizing our process to prioritize the appropriate patients for this investigational drug in accordance with the emergency use criteria defined by the FDA.
Very soon, we will start administering this new treatment that helps limit the amount of virus in the body to those patients identified as most likely to benefit. Studies indicate the drug is most effective when COVID-19 patients receive it within 10 days of symptoms starting.
If you or a loved one are experiencing symptoms of COVID-19, it’s important to act fast. Visit baptisthealth.com/covid-19 for treatment and testing options, and to learn more about this virus.

Get health tips, treatment, and evaluation on your schedule with Baptist Health.
Find a ProviderFDA
UPMC
Helpful Resources and Next Steps:
Convalescent Plasma Therapy
What is the COVID-19 Vaccine?
COVID-19 Article Library
[Podcast] COVID-19: What You Need to Know